Difficult emotions: understanding emotional dysregulation in complex post-traumatic stress disorder (cPTSD).
- Difficult emotions: understanding emotional dysregulation in complex post-traumatic stress disorder (cPTSD).
- I. Introduction
- A. Emotional dysregulation in cPTSD: understanding the basics
- B. What is cPTSD: an overview
- C. Why it is important for people with cPTSD to seek help for emotional dysregulation.
- II. Emotional dysregulation in cPTBS
- A. Emotional dysregulation in cPTSD: recognizing the signs
- B. Emotional dysregulation in cPTSD: the impact on everyday life and relationships
- III. Causes of emotional dysregulation in cPTBS
- A. Emotional dysregulation in cPTSD: the role of trauma and stress
- B. Emotional dysregulation in cPTSD: the neurobiological causes
- C. Emotional dysregulation in cPTSD: genetic predisposition
- IV. Effective treatments for emotional dysregulation in cPTBS
- A. How psychotherapy can help overcome emotional dysregulation in cPTBS
- B. Medication: a complementary approach to treating emotional dysregulation in cPTBS
- C. Mindfulness and self-care: the power of self-care in managing emotional dysregulation in cPTBS
- Self-care: Managing emotional dysregulation
- The window of tolerance
- Expanding your tolerance window
- Increase your stress tolerance
- Explore and feel
- How am I doing?
- V. Conclusion: Help for emotional dysregulation in cPTBS
- A. A brief summary of the importance of understanding emotional dysregulation in cPTSD.
- B. Treatment for emotional dysregulation in cPTSD is important
- VI. Sources
All people who have grown up in abuse and neglect have difficulty expressing their feelings. They easily lose their temper, cry uncontrollably and feel out of control, or they shut down and feel cut off from their feelings. Both patterns are examples of emotional dysregulation that make life difficult for people with cPTSD.
I. Introduction
A. Emotional dysregulation in cPTSD: understanding the basics
Emotional dysregulation refers to difficulty in controlling and regulating emotions. It is characterized by intense and unstable mood swings, irritability, outbursts of anger and a tendency to overreact to triggers. Emotional dysregulation can cause significant stress and interfere with daily life and relationships.
B. What is cPTSD: an overview
Complex post-traumatic stress disorder (cPTSD) here refers to a condition that can develop in children after experiencing repeated abuse or neglect over an extended period of time. cPTSD is characterized by a range of symptoms, including emotional dysregulation, relationship and trust problems, toxic feelings of guilt and shame, and a persistent sense of emotional numbness.
C. Why it is important for people with cPTSD to seek help for emotional dysregulation.
With good affect regulation, you feel grounded and calm. You can compassionately accept that difficult emotions are an inevitable part of life. You can express a range of emotions without feeling overwhelmed, numb or addicted to harmful behaviours. Affect regulation enables you to make healthy choices, advocate for your needs and communicate successfully with others. In contrast, disorders of affect regulation mean that you experience uncontrollable sadness, anger or anxiety that interferes with your concentration at work, interactions with your children or loving relationships. You may be afraid of being abandoned. Or you may feel triggered by the behaviour of others or distressed when someone you care about is disappointed in you. Emotional dysregulation often leads to behaviours that you later regret. For example, you may take your anger out on others or feel the urge to hurt yourself. These behaviours often lead to a vicious cycle of guilt and self-loathing, from which suicide may eventually appear as the only way out of your pain.
This post helps to provide an in-depth understanding of emotional dysregulation in cPTSD. It explores the nature of emotional dysregulation, its causes and the treatment options available to manage this distressing symptom. It aims to educate people struggling with emotional dysregulation and provide them with the information they need to find help and support.
II. Emotional dysregulation in cPTBS
A. Emotional dysregulation in cPTSD: recognizing the signs
Emotional dysregulation in cPTSD can manifest itself in rapid and intense mood swings, irritability, outbursts of anger and a tendency to overreact to triggers. These emotions are overwhelming and difficult to control, causing significant distress. People with cPTSD may also struggle with anxiety and depression, which can exacerbate the symptoms of emotional dysregulation.
B. Emotional dysregulation in cPTSD: the impact on everyday life and relationships
Emotional dysregulation can have a significant impact on daily life and relationships. Intense and unstable mood swings can cause difficulties in maintaining stable relationships and lead to social isolation. Emotional dysregulation can also lead to harmful coping mechanisms such as substance abuse, self-harm and other harmful behaviours.
III. Causes of emotional dysregulation in cPTBS
In childhood, we learn how to control our emotions. Children need healthy, caring and attentive adults to help them develop their social and emotional intelligence. It is the job of parents to make sure that children feel safe enough to express uncomfortable feelings. When children feel supported, they learn that stressful moments are temporary and can lead to positive experiences of self-determination or deepened relationships. However, emotionally overwhelmed parents fail to help their children achieve a healthy landscape of emotions. Instead, affects become mined territory – children become explosive or cut off from their feelings. In some cases, children become hyper-aware of their parents’ distress or are forced to attend to their parent’s emotional needs.
A. Emotional dysregulation in cPTSD: the role of trauma and stress
The most important cause of emotional dysregulation in cPTSD is trauma and stress. Prolonged experiences of traumatic events and stress can lead to brain and nervous system changes that result in emotional dysregulation. These changes can affect the regulation of emotions and the ability to cope with stress, leading to intense and unstable mood swings.
B. Emotional dysregulation in cPTSD: the neurobiological causes
Trauma and stress can cause brain structure and function changes, leading to emotional dysregulation in cPTSD. Repeated exposure to traumatic events can change how the brain processes emotions, resulting in overreaction to triggers and intense emotional responses. In addition, there may be dysregulation of the nervous system, leading to an increased physiological response to stress and a heightened state of arousal.
C. Emotional dysregulation in cPTSD: genetic predisposition
There is also evidence that a genetic predisposition may play a role in developing emotional dysregulation in cPTSD. Certain genetic factors may increase a person’s vulnerability to stress and trauma, making them more likely to develop emotional dysregulation due to traumatic events. However, it is essential to note that genetics can only partially explain the development of emotional dysregulation and that a combination of genetic, environmental and psychological factors are likely to be involved.
IV. Effective treatments for emotional dysregulation in cPTBS
A. How psychotherapy can help overcome emotional dysregulation in cPTBS
Psychotherapy is an effective treatment for emotional dysregulation in cPTSD. Trauma-focused therapies, including cognitive behavioural therapy (CBT) and eye movement desensitization and reprocessing (EMDR), can help sufferers regulate their emotions and reduce the impact of traumatic memories. These therapies also help sufferers develop better coping strategies, improve their self-esteem and strengthen their relationships.
B. Medication: a complementary approach to treating emotional dysregulation in cPTBS
Medications such as selective serotonin reuptake inhibitors (SSRIs) and mood stabilizers can also effectively treat emotional dysregulation in cPTSD. These medications can help regulate mood swings and reduce the intensity of emotional reactions. However, medications are only one component of a comprehensive treatment plan.
C. Mindfulness and self-care: the power of self-care in managing emotional dysregulation in cPTBS
Self-care: Managing emotional dysregulation
In this section, you will learn skills to help you develop a healthy imbalanced relationship with difficult emotions. You can also use these tools to enrich your inner life and increase your capacity for joy.
The window of tolerance
Patterns of behaviour learned in childhood can develop in adulthood into uncontrollable outbursts of tears or anger, feelings of lethargy or dullness, or overly intense reactions to the feelings of others. These patterns of emotional dysregulation indicate that you are outside your “tolerance window” – a term coined by Dr Dan Siegel to describe the range of stress that a person can manage without overexertion. Within the tolerance window, we can successfully deal with distressing feelings and stressful experiences and physical sensations. Within our tolerance window, we can manage stress and return to a sense of safety.
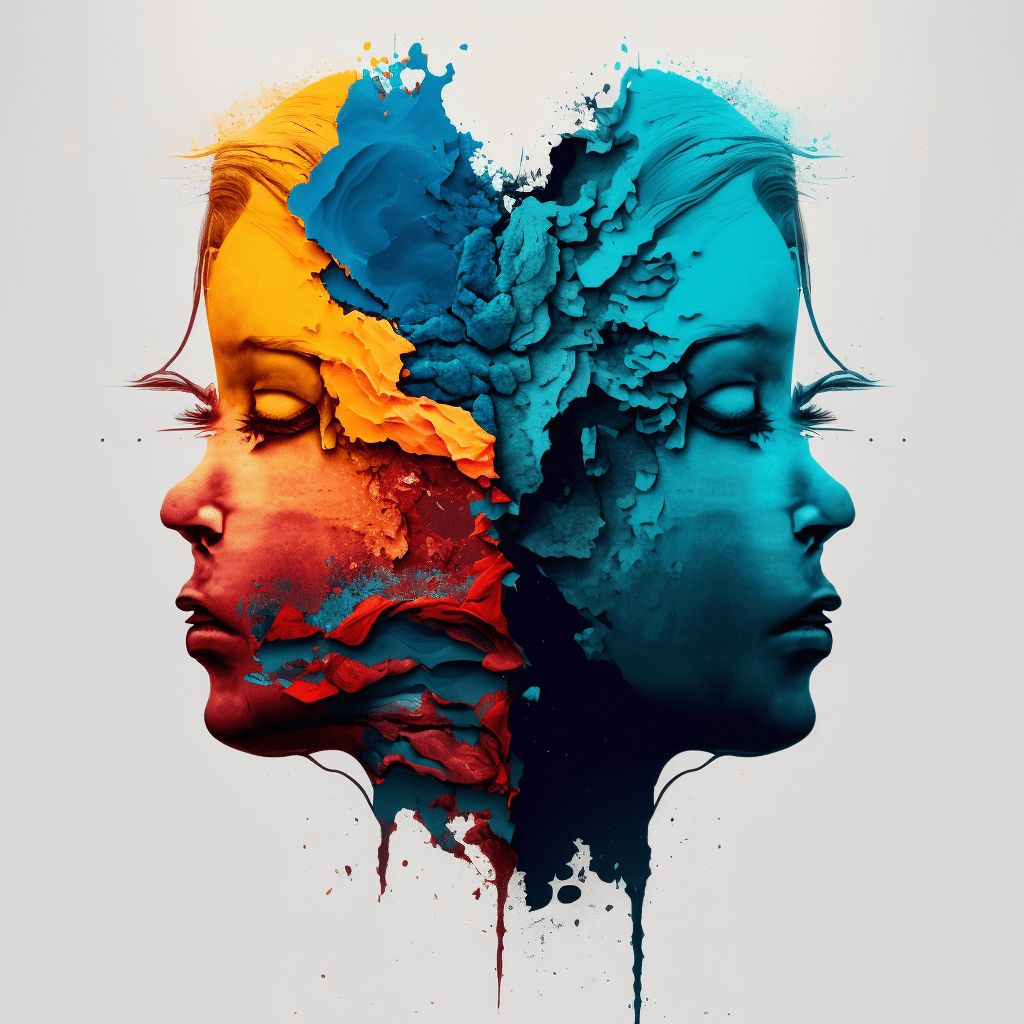
Outside the tolerance window, emotions such as anxiety, irritability, restlessness, anger or sadness build up to high levels. Our sympathetic nervous system jumps on. In contrast, low arousal emotions mean a reaction from the parasympathetic system. We may feel tired, lethargic, helpless, emotionally dulled, numb or depressed. People with cPTSD often alternate between these highs and lows. The patterns of dysregulation learned in childhood often continue into adulthood. They form the individual pattern of the 4 Fs: attack, flight, play dead or submission.
Fight reactions lead to criticism of oneself and others, anger and rage. A pronounced need for control also belongs here.
Flight reactions are jumpiness and constant vigilance. You may feel rushed, “trapped in your head”, experience racing thoughts or feel disconnected from your body. You may be running from memories of the trauma.
When a child learns to attend to a parent’s emotional needs, he or she relies on a fawning response – an attempt to appease or please an aggressor, to meet his or her emotional needs, to prevent an attack. This submissive response often leads to an enmeshed attachment to the offender. In adulthood, such unresolved patterns can lead to co-dependency, where one sacrifices one’s own needs to maintain relationships.
“Playing dead”, a freeze reaction, occurs when you remain absolutely motionless in the expectation that your life is threatened. You hold your breath and are paralysed. This can go as far as fainting when our body decides that we are threatened and must conserve energy to survive. First, we feel distant, alienated, and numb and have the urge to withdraw from others – dissociation occurs. Then come nausea, dizziness, loss of balance, and even clouding consciousness.
Expanding your tolerance window
First, it is crucial to learn to stay within our tolerance window. After that, overcoming trauma will strengthen overall emotional resilience. The tolerance window expands.
You can widen your tolerance window by paying compassionate attention to unpleasant emotions and bodily sensations while acknowledging that these feelings do not require a reflexive response. For example, you might notice a feeling of irritability, a change in breathing, a loss of concentration or a sudden tiredness. But, instead of repressing these feelings, you curiously approach them inwardly (REST). You may discover that these feelings have something to do with the past. Maybe your body is letting you know that you need to change something. Instead of reacting impulsively now, you can choose positive coping strategies and wiser behaviours such as setting a boundary, standing up for yourself or mindfully ending an unhealthy relationship.
Do you see anything that matches your own patterns of emotional reactions? This self-knowledge will help you work with affect regulation. Remember that growth requires patience. Be gentle and understanding with your feelings and sensations, and proceed at a pace that does not overwhelm you. Learn to live with discomfort without fear. This way, you expand your tolerance for unpleasant affects and get in touch with your physical sensations. This is the basis for positive changes, such as more self-compassion and improvements in your relationships with others.
Increase your stress tolerance
An essential goal of therapy is to learn how to deal successfully with painful feelings. No one can escape the challenges that come with being human. Unpleasant sensations or emotions often accompany them with habitual thoughts of, “Make this go away!”, or, “I can’t stand this!” These thoughts can lead to self-harming behaviours: explosive emotional outbursts or the urge to use drugs.
Stress tolerance is an exercise in mindfulness. Proceed as you would in sitting meditation. Set a five-minute timer, so you don’t have to look at the clock. Sit comfortably on a chair or a cushion on the floor.
Start so that you can observe your sensations and feelings. If you notice an uncomfortable feeling, glide, curious. Do not give in to the urge to push the sensation or feeling away. Know that feelings do not last.
Instead of judging your experience, describe your sensory perceptions to yourself. Pay attention to your sensations of warmth or cold, areas of tension in your body, the feeling in your hands or the sensation of your breath. Observe what happens if you dwell with emotion a little longer.
Notice any slight changes that occur as you continue to breathe and observe your experience. You may find that distress subsides through mindful, reflective observation. You may find that you can consciously turn to the underlying emotions and resolve them.
Explore and feel
Explore how to address your body when you feel emotionally overwhelmed or shut down. Practice each of these encouraging movements mindfully and slowly. Repeat each movement two or three times, then pause to feel subtle changes in your body and mind.
● Stand next to a wall and press your arms firmly against the wall. Press and release several times. Imagine setting a boundary and pushing away everything you don’t want or that threatens you.
● Stand up and walk slowly and mindfully in place. Imagine that you are leaving an unpleasant situation.
● While sitting or standing, press your feet into the ground, tense the big leg muscles, and then relax. Stand firm and know that no one can push you over.
● Stretch your arms out in front of you as if you are reaching for something important to you. Feel how it feels to reach for what you want.
● Imagine holding what you want in your hands and pulling your arms back towards your chest. Explore how it feels to receive.
● When you feel emotions, pay attention to the accompanying sensations in your body. Notice how it feels when you place your hands on these sensations, apply light pressure, and breathe deeply.
● When you sit down, allow yourself to rest in your connection with your chair or couch. Pay attention to whether you feel the urge to collapse. If so, see if you can build enough muscle tension to feel relaxed and awake.
How am I doing?
Take a moment, pause and reflect. Did this post activate or trigger anything?
Think about a current challenge. As you do, notice subtle changes in your belly, chest or throat. Do you notice small changes in your breathing? Instead of ignoring these signals, ask yourself: what is my body trying to tell me? Experiment. Over time, figure out how your body, mind and emotions work together.
Other mindfulness and self-care practices such as meditation, yoga and regular exercise can also help sufferers manage the symptoms of emotional dysregulation in cPTSD. They reduce stress and increase overall well-being, leading to better affect regulation. In addition, regular practice of self-care activities can help sufferers develop better coping strategies and reduce the impact of trauma on their daily lives.
V. Conclusion: Help for emotional dysregulation in cPTBS
A. A brief summary of the importance of understanding emotional dysregulation in cPTSD.
This post discusses emotional dysregulation in cPTSD, its characteristics, causes and effective treatment options. We highlighted the importance of understanding that emotional dysregulation is a symptom of cPTSD, not a character flaw or weakness. We also discussed the relationship between trauma, stress and brain changes and their role in emotional dysregulation development.
B. Treatment for emotional dysregulation in cPTSD is important
Effective treatment options such as psychotherapy, medication, mindfulness and self-care can help people manage their symptoms and improve their overall well-being. With the right support and treatment, people with cPTSD can learn to regulate their emotions, reduce the impact of trauma and improve their daily lives and relationships.
For those affected by childhood trauma who struggle with emotional dysregulation and cPTSD, seeking help can be challenging. But remember that emotional dysregulation is a treatable condition. With the right support and resources, sufferers can make significant progress. For their personal growth, sufferers can turn to a therapeutic facility or join a support group. Mindful self-care is important to manage symptoms and improve overall well-being. Remember: you are not alone, and help is available.
VI. Sources
- National Center for Posttraumatic Stress Disorder. (2021). Complex PTSD. Retrieved from https://www.ptsd.va.gov/professional/treatment/overview/complex-ptsd.asp
- American Psychological Association. (2021). Eye Movement Desensitization and Reprocessing (EMDR). Retrieved from https://www.apa.org/ptsd-guideline/treatments/eye-movement-desensitization-reprocessing
- National Institute of Mental Health. (2021). Selective Serotonin Reuptake Inhibitors (SSRIs). Retrieved from https://www.nimh.nih.gov/health/topics/depression/selective-serotonin-reuptake-inhibitors-ssris
- American Psychological Association. (2021). Cognitive Behavioral Therapy (CBT). Retrieved from https://www.apa.org/ptsd-guideline/treatments/cognitive-behavioral-therapy
- National Center for Complementary and Integrative Health. (2021). Mindfulness Meditation. Retrieved from https://www.nccih.nih.gov/health/mindfulness
- American Psychological Association. (2021). Self-Care for Mental Health. Retrieved from https://www.apa.org/helpcenter/self-care
- World Health Organization. (2021). Mental Health: Trauma and Stress-Related Disorders. Retrieved from https://www.who.int/mental_health/management/trauma_stressor-related_disorders/en/
- Schwartz, A. (2016). The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control and Becoming Whole. Althea Press.
- Schwartz, A. (2020). A Practical Guide to Complex Ptsd: Compassionate Strategies to Begin Healing from Childhood Trauma. Rockridge Press.
- Walker, P. (2013). Complex PTSD: From Surviving to Thriving: A Guide and Map for Recovering from Childhood Trauma. CreateSpace.
- Walker, P. (2015). The Tao of Fully Feeling: Harvesting Forgiveness Out of Blame. Createspace Independent Publishing Platform.